EPILEPSY SURGERY
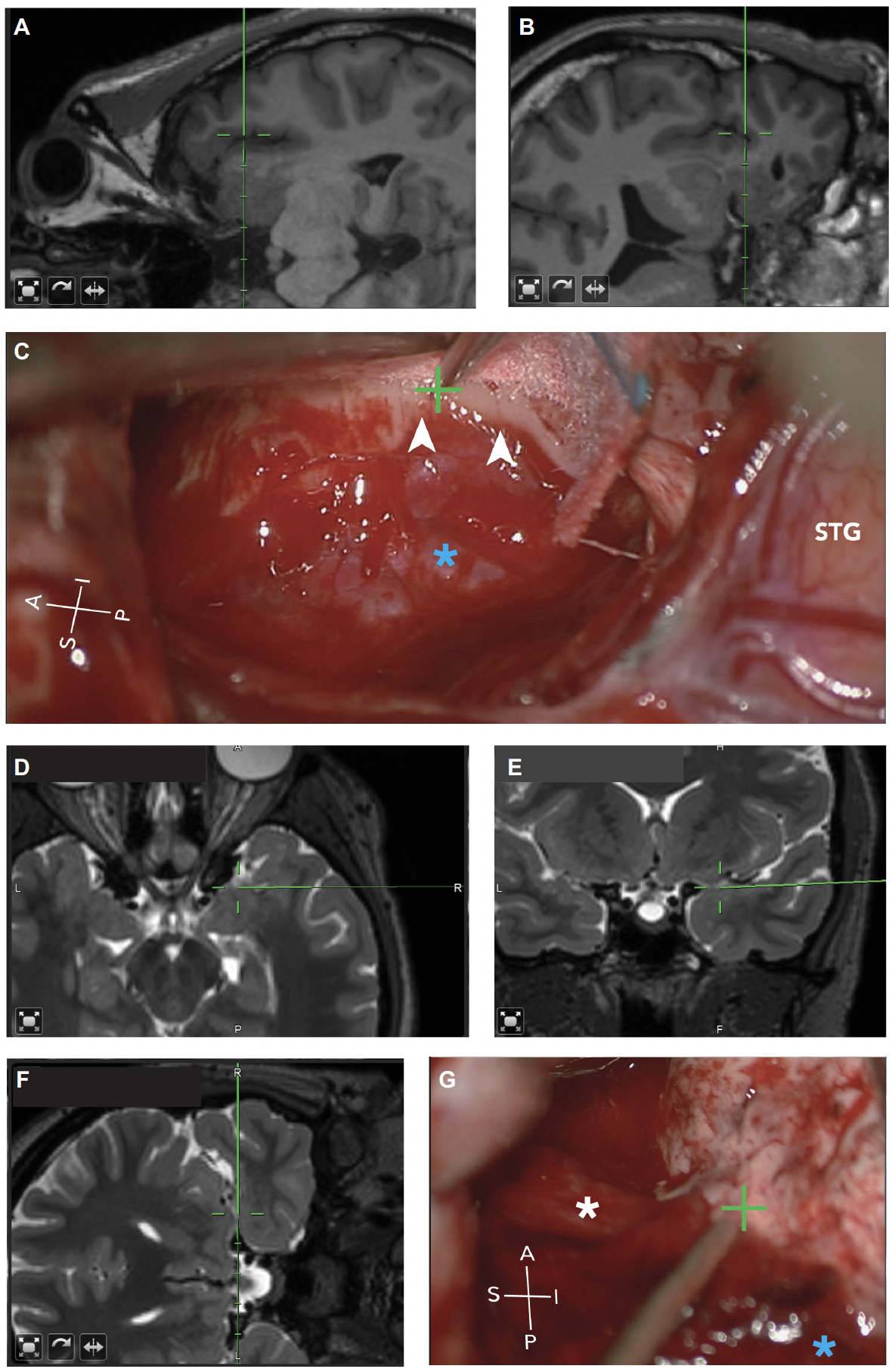
The Brain Modulation Lab has contributed to advancing both resective and neuromodulatory surgical approaches for drug-resistant epilepsy. In the domain of temporal lobe epilepsy surgery, we developed and reported a standardized extrapial hippocampal resection technique for anterior temporal lobectomy, demonstrating in a 62-patient case series that this approach yields seizure freedom rates of 79% (follow-up <3 years) and 52% (follow-up >3 years), with a low complication rate and consistent recovery of en bloc hippocampal specimens suitable for translational research (Hussein et al., Operative Neurosurgery, 2021). We also demonstrated that intracranial monitoring equalizes seizure outcomes in patients with nonconcordant presurgical data, with SEEG being the only approach used for bilateral or poorly lateralized temporal lobe epilepsy and resulting in 77.8% seizure freedom, notably with 85% of SEEG patients having their primary surgical hypothesis modified by the intracranial data (Sokolov et al., Epilepsia Open, 2022). Mike Modo’s lab at the University of Pittsburgh leveraged en bloc hippocampal specimens generated by the extrapial technique, to perform ex vivo mesoscale diffusion MRI that bridges the gap between macroscopic imaging and microscopic histopathology. This work began with the first demonstration that aberrant mossy fiber connections (a putative substrate for reverberant excitatory circuits in mesial temporal sclerosis) could be visualized using mesoscale diffusion MRI with histological validation (Modo et al., Human Brain Mapping, 2016), followed by systematic optimization of acquisition parameters for mesoscale hippocampal imaging (Ly et al., Human Brain Mapping, 2020) and the finding that intra-hippocampal diffusion metrics correlate with preoperative seizure frequency, providing a potential microstructural biomarker linking tissue pathology to clinical severity (Ke et al., Human Brain Mapping, 2020).
Our lab has been at the forefront of developing thalamic responsive neurostimulation (RNS) as a therapeutic strategy for drug-resistant epilepsy, beginning with the first use of bilateral centromedian (CM) thalamic RNS in a patient with idiopathic generalized epilepsy (IGE) in 2017. That index patient, a young woman with drug-refractory Jeavons syndrome (eyelid myoclonia with absences), experienced a reduction in daily absence seizures from a mean of 60 to fewer than 10, and notably retained awareness during residual episodes (Kokkinos et al., Neurosurgery, 2020). We subsequently reported an initial case series of four patients with pharmacoresistant IGE who underwent bilateral CM-region RNS implantation, achieving 75%–99% reductions in seizure frequency with decreased seizure duration and severity, and significant improvements in quality of life that were durable through at least two years of therapy (Sisterson et al., Journal of Neurology, Neurosurgery & Psychiatry, 2022). Most recently, we expanded this work in a multicenter cohort of 21 patients with drug-resistant generalized and multifocal epilepsy, including focal-to-bilateral tonic-clonic seizures, demonstrating an average seizure reduction of 82.6% for patients with at least one year of follow-up, with 18% achieving Engel class 1 outcomes and no patients classified as Engel class 4 (Nanda et al., Epilepsia, 2024). Our clinical collaborators also demonstrated the emergent use of RNS in the acute treatment of super-refractory status epilepticus, reporting the first case of focal motor epilepsia partialis continua successfully treated with responsive neurostimulation when all conventional medical interventions had failed (Yang et al., Annals of Clinical and Translational Neurology, 2021). Collectively, this body of work has contributed to a growing recognition that thalamic RNS can extend surgical treatment to patients with generalized and multifocal epilepsy who were not previously considered candidates for intracranial neuromodulation.
Our work has also advanced the broader conceptual framework for epilepsy surgery. Dr. Richardson has articulated a paradigm shift from traditional focus-oriented surgical philosophy to a network-oriented approach, explaining that all patients with drug-resistant epilepsy are potential surgical candidates and that stereoelectroencephalography (SEEG) should be reconceived as a network-discovery platform that informs both resective and neuromodulatory strategies (Richardson, Neurological Clinics, 2022). We further contributed to the field's understanding that epilepsy surgery, including neuromodulation, can improve not only seizure control but also neurodevelopment in children with epileptic encephalopathies, providing evidence that surgical intervention should be considered earlier in the disease course to maximize cognitive outcomes (McLaren et al., Neurosurgery Clinics of North America, 2024). He further explained that hypothesis-driven thalamic SEEG should be integrated into routine clinical practice — rather than treated as research — to enable individualized identification of optimal neuromodulation targets, given that empirical data now demonstrate substantial and durable seizure reduction across multiple thalamic nuclei (Richardson, Brain, 2026).
Across these lines of investigation, our program has sought to broaden the scope of who is considered a surgical candidate and how surgical decisions are made. Together with the conceptual shift toward network-oriented epilepsy surgery, these efforts address a longstanding problem in the field: epilepsy surgery remains substantially underutilized despite strong evidence of efficacy, in part because many patients with drug-resistant epilepsy do not fit the traditional model of a resectable focal lesion. By expanding both the technical repertoire and the conceptual framework for surgical intervention, this body of work contributes to ongoing efforts to close the treatment gap for patients with medically refractory epilepsy.